Sudden Infant Death Syndrome (SIDS) and Sudden Unexpected Infant Death (SUID) are horrific things, but there are actionable steps parents can take to decrease risk. In October 2016, the American Academy of Pediatrics (AAP) released updated recommendations on reducing risk. But here’s the thing: many parents and prospective parents didn’t hear about these updated, potentially life-saving guidelines. Notably new for 2016 is the recommendation children sleep in the same room (though a different sleep surface) as parents for at least 6 and ideally 12 months.
We conducted a poll of parents and prospective parents in December 2016 and found that 76% of parents did not know when the AAP last updated SIDS guidelines – the word on these important guideline changes is just not getting out to the right folks.
In addition, the AAP published a study in September of 2016 that found
- 10%-21% of parents put children on an unsafe surface,
- 14%-33% of parents put children to sleep in an unsafe position
- 87%-93% of parents allowed unsafe items nearby their child
We’re on a mission to get these recommendations into the hands of as many people caring for infants as possible, and we very much hope you’ll help by sharing this post and our related Facebook video. You can click or tap on a share button for your favorite social network to help spread the word.
Let’s Get Started
First, a note. THIS IS SERIOUS SHIT PEOPLE. We’ve researched this extensively and are using the most reputable sources out there, but WE ARE NOT DOCTORS. ONLY YOU ARE RESPONSIBLE FOR YOUR CHILD’S WELLBEING. IF YOU HAVE QUESTIONS, CONSULT YOUR CHILD’S PEDIATRICIAN.
Today we’re going to talk about SIDS and similar causes of sleep-related infant death. We’re fully aware that this topic is so awful to consider it may be tempting to retreat to happier/friendlier/funnier corners of the internet filled with cat photos and the like. Please don’t. With just a few minutes of education and a few simple changes, you can reduce the risk of SIDS for the small, lovable folks in your life.
So, in service of presenting some cuddly creatures, we created this video demonstrating some important SIDS & SUID risk-reduction factors using stuffed polar bears.
You also may feel like you already know about SIDS and how to reduce the risk, but did you know that in October 2016 the American Academy of Pediatrics released updated SIDS guidelines? We surveyed parents and parents to be of small kids and found that while 100% of respondents had heard of SIDs and 86% were taking measures to reduce risk, only 24% of them had seen the updated guidelines. Even if you think you know the latest, this is worth a quick refresher.
So pay attention because you can reduce the risk of SIDS, which is the leading cause of death in infants under the age of 12 months.
TL;DR / For Visual Learners
We don’t recommend you skim or skip parts of this post. It’s not that long and this is important. But, we recognize you may be holding your sleeping infant while balancing on one foot in a crowded subway car because this is the only way you can get her to fall asleep (we don’t recommend this either). So, we present our visual guide to understanding SIDS (click to enlarge):
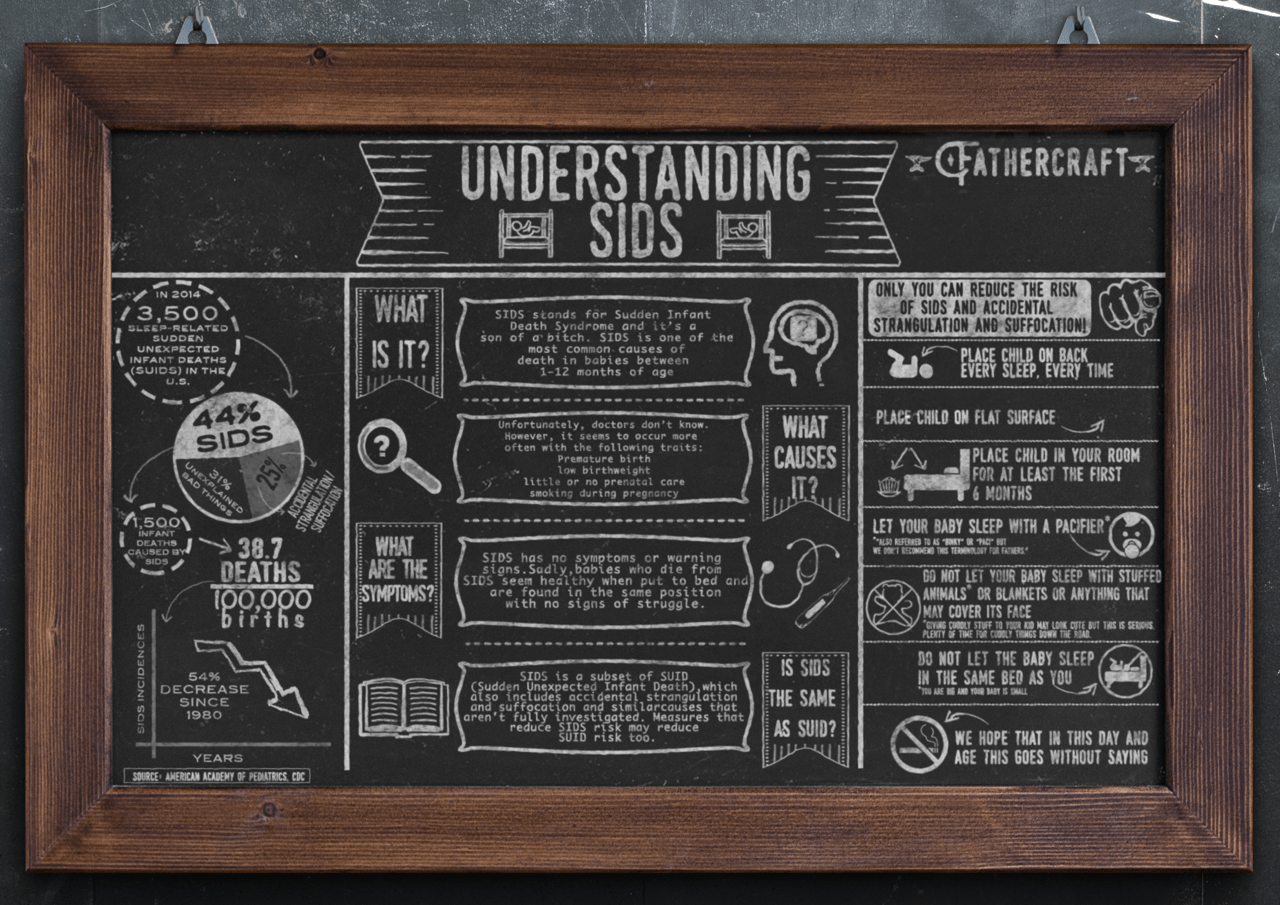
What is SIDS?
SIDS stands for Sudden Infant Death Syndrome. It’s part of a larger family of causes of death in infants less than one year of age called SUID – Sudden Unexpected Infant Deaths. All forms of SUID occur while a child is sleeping, and are broken down like this:
Accidental Strangulation and Suffocation. Occurs when an infant suffocates or is strangled during sleep, as a result of 1) being smothered by soft bedding, a pillow or blanket covering the infant’s nose and mouth, another person rolling on top of the infant while asleep, becoming wedged or trapped in between objects (ie. mattress and wall or bed frame or 2) being strangled, for example when the infant’s neck becomes trapped between crib railings.
SIDS. Occurs when, after an investigation is conducted, the cause of death cannot be determined (i.e. not accidental strangulation and suffocation).
Unknown Cause. When an infant dies in his or her sleep, but a thorough investigation cannot be completed. If it were, these deaths would likely be attributed to SIDS or accidental strangulation/suffocation.
The CDC notes even after a detailed investigation, it can be difficult to classify SUID into its different forms. Fortunately, the preventative measures recommended by leading researchers and organizations are designed to reduce risk across all forms of SUID.
What Causes SIDS and SUID?
By definition, doctors and scientists are unsure what causes SIDS – it is diagnosed when an infant dies in her sleep and no other cause can be determined. Recently, researchers in Australia have made important discoveries that may lead to a deeper understanding of the causes, and potential screening techniques to further reduce SIDS deaths.
A variety of factors cause, and are thought to cause, SUID deaths. The most well-understood of these are factors leading to smothering and strangulation.
Smothering caused by:
- pillow
- mattress
- stuffed animal
- loose clothing worn to sleep covering the infant’s face, nose or mouth
- another person sharing a bed with the infant
- Other hazards in the sleep area
Strangulation caused by the infant’s head or neck being trapped
- between crib bars
- between a mattress and a wall
- between a mattress and crib railings
- other hazards in the sleep area
What Can You Do to Reduce the Risk?
The CDC, the American Academy of Pediatrics, and other world health authorities recommend a number of measures to reduce the risk of SIDS and SUID, which we’ve outlined below. A couple of notes here:
- Do the work. Read directly from the CDC here, and directly from the APP here.
- A number of these recommendations seem over-the-top or seem to deprive your child – it is recommended that you do not give your child any stuffed animals, any soft blankets, and that your child’s sleeping surface be very firm (no foam mattresses, pillowtops, etc.) So basically nothing that seems like it would make your infant cute and comfortable. We know this sounds harsh, but all these recommendations are made for the safety of your child by leading health organizations. There will be plenty of time for snuggly blankets and cute stuffed animals down the road.
- Manufacturers and reputable stores may get it wrong. Don’t assume that because your favorite store is selling crib bumpers or stuffed animals that are suitable from birth this means they’re ok to give your child during sleep.
Measures to Reduce SIDS and SUID Risk
Place your infant on her back to sleep, every time. Unless your doctor has discussed otherwise with you, put your child to sleep on her back, not her stomach. Experts have determined this is the safest position for children under one year of age to sleep. A common concern heard about back to sleep is, ‘What if my child vomits? Couldn’t they choke on their own vomit?’. It’s a reasonable concern, but infants have a reflex that causes them to turn their head when they vomit.
Place your infant on a flat, firm surface. A crib with a flat, firm mattress is the safest place for your baby to sleep. A firm mattress reduces the risk of suffocation if the infant rolls over in her sleep, and a flat surface allows airways to remain fully open. It is also for this reason that experts do not recommend that children sleep in car seats or other places that cause them to be in a hunched-over position.
Place your child’s crib in your room for at least the first 6 months of life. This recommendation is new from the APP for 2016 – proximity to you and your partner allow you to use visual and auditory signals to check on your infant. That nursery you’ve prepared? It should wait.
Let your baby use a pacifier. In addition to being helpful for soothing, researchers believe pacifiers may reduce SIDS risk.
Do not allow stuffed animals, pillows, or blankets in the crib. All of these items, plus anything soft or with the ability to cover your infant’s mouth or nose, should be avoided.
Don’t share a bed with your baby. So-called “co-sleeping” is popular in some circles, but your bed is too soft, and you are at risk for rolling over on your infant and suffocating them while you’re asleep.
Don’t use crib bumpers. Cute but also unsafe. Also unnecessary – your baby isn’t going to roll over and bump his head on the crib bars with enough force to do anything harmful.
Don’t expose your child to secondhand, or even thirdhand smoke. This should go without saying, but even thirdhand smoke (you are around someone who is smoking, then come home to your baby with smoke on your clothes, in hair, etc. should be avoided. Take a shower and change if you find yourself around smokers.
Stop swaddling your child when she can roll over. Once your child is able to roll over on her own, experts recommend you stop swaddling to prevent your child from getting stuck on her stomach or rolling into the side of a crib and becoming trapped.
Other recommendations include: avoid alcohol* and illicit drug use during pregnancy and while breastfeeding, breastfeed your child if possible, avoid overheating your child by putting them in too many layers of clothing or in a room that’s too warm, do not use weighted blankets.
Now that we’ve covered the recommendations, let’s jump into some FAQs about SIDS & SUID
Frequently Asked Questions: SIDS & SUID
If you’re like most parents, you probably have a ton of questions about SIDS & SUID. Because there are still some unknowns surrounding the realities of sudden infant deaths, it’s important to stay informed of the latest research. Keep up to date on the guidelines from the American Academy of Pediatrics and talk to your pediatrician if you have any questions. That said, here are some FAQs we frequently encounter:
Q: What is the peak age for SIDS?
According to the American Academy of Pediatrics, infants are at a heightened risk of SIDS between the ages of 1 month and 4 months old. However, items like soft bedding continue to pose a danger even beyond four months of age. Some people might be surprised to learn that SIDS risk lasts until the baby is at least 12 months old.
This long time frame of SIDS danger explains why the AAP recommends sleeping in the same room as your baby for at least 6 months, but preferably an entire year. So, even if you have that nursery decorated to the nines, you might choose to have your baby sleep in the same room as you for longer than you anticipated.
Q: At what age does SIDS & SUID risk go down? Why?
The National Health Institute provides an interesting infographic on the time frame of SIDS and SUID, highlighting that 72% of infant deaths occur before 4 months and 90% occur before 6 months of age. After this, SIDS risk goes down dramatically (comprising the remaining 10%) – though still remains possible until your baby’s first birthday.
So, why does this risk decrease so dramatically after 6 months of age? Although there is some scientific uncertainty surrounding SIDS, the reason for the drop-off rate could have something to do with increased motor skills developing by 6 months of age. Sure, 6-month-old babies still need a lot of help, but by this time many of them are capable of holding their own weight in a standing position, roll from their back to their stomach, and can even lift their own chest and head when on their stomachs.
Q: Should weighted blankets be used for infants?
No, absolutely not. Let’s elaborate.
You may have come across weighted blankets at some point during your child-supplies research. Stuffed with things like flax or other natural materials, weighted blankets can be a useful device for providing comfort for older children with sensory disorders. The key in this situation is that these blankets are only appropriate for older children and adults.
Weighted blankets have been implicated in tragic deaths for infants. Once again, there should not be anything in the baby’s crib that could pose a risk of strangulation or suffocation: soft bedding, blankets, pillows, wedges, bumpers, and stuffed animals are eall out. It’s best to use a wearable blanket for baby, as it stays nice and snug to their bodies. Just remember that SIDS is linked to over-bundling and overdressing, and make sure your baby is in no danger of overheating.
Q: Can swaddling cause SIDS?
The American Academy of Pediatrics does not recommend against swaddling your baby. However, they also say that there is no evidence that swaddling decreases the risk of SIDS. An important caveat: the AAP states there is a “strong risk of death” for a swaddled infant that is placed in the prone position (on their tummy) or who rolls to the prone position. If you always put your swaddled infant on her back to sleep, then this risk is certainly decreased. Once your baby starts to roll over on her own, swaddling is no longer safe.
Before your baby can roll over, you can swaddle her: just make sure it is snug around her chest, but not too tight around her hips. Again, once your infant shows signs of rolling (which can happen as early as 3 or 4 months old) then discontinue swaddling. In addition, don’t over-bundle the baby, and never cover his face while he is sleeping (or awake.)
We’ll state again that improper swaddling can increase SUID risk as loose materials over a baby’s mouth, nose and face can reduce airflow to your baby. It’s for this reason many experts recommend using sleep sacks instead of swaddling manually with a blanket. Our favorite? The Sleepea from Happiest Baby — you can check out our review here.
Q: Can SIDS/SUID happen while holding your baby?
It’s so important for both moms and dads to enjoy skin-to-skin with infants, and there’s nothing cozier than cuddling your little bundle of joy. However, there’s a risk of SIDS when parents (generally exhausted parents) fall asleep while holding their baby. It’s for this reason that the AAP recommends that you avoid sitting on sofas, recliners, or comfy chairs if there’s any risk you might fall asleep while holding your little one. Similarly, never place your baby down to sleep on any surface that isn’t a firm mattress specifically designed for babies – this presents an “extremely hazardous” situation, according to the AAP.
Unfortunately, what happens in some cases is that the baby becomes wedged in the sofa and suffocates. So, hold your baby whenever you are conscious, awake, and able to respond appropriately. But if you need to sleep or even just rest your eyes for a moment, put your baby down on their back on a firm surface.
Q: Can SIDS happen while a baby is awake?
In the vast majority of cases, SIDS occurs when the baby is sleeping. This is likely linked to babies being placed in improper sleeping positions or other environmental factors, However, there are also some physical factors that can contribute to SIDS in waking babies. For example, a baby may have brain defects in the area of their brain that governs breathing. Or babies might have compromised respiratory systems because of a recently-acquired cold.
Again, it is extremely rare for an infant to die from SIDS while awake. Think about it – while your infant baby is awake, you are probably awake as well and ready to respond to their needs.
Wrapping Up
If you are making all the right choices, following the AAP’s guidelines, and staying alert, then there’s no need to live in a constant state of anxiety about SIDS & SUID. Just remember that parental lifestyle choices count: quit smoking and avoid drugs and alcohol when your kids are infants. Always put your baby to sleep on her back, in a crib, and never keep loose items in her crib or bassinet.
Thanks for taking the time to better understand SIDS and SUID and what you can do to reduce the risk. We greatly appreciate that you care about children’s safety as much as we do, and would love it if you could share this post with others. Just click or tap your favorite share button to share with those you care about.
*Some experts believe alcohol in moderation (ie one glass of wine or one beer on occasion) is ok during pregnancy and breastfeeding. This is a deeply personal choice and we leave this research, and decision making, to you.
Sources
https://www.cdc.gov/sids/about/index.htm
https://pediatrics.aappublications.org/content/138/5/e20162938
https://www.telegraph.co.uk/news/2016/11/16/end-of-sids-in-sight-australian-researchers-make-breakthrough-in/
https://www.aappublications.org/news/2016/08/15/SafeSleep081516